This blog post provides a thorough overview of the main challenges encountered during breastfeeding and practical solutions. Here, you'll find useful information for both your and your baby's comfort.
Latch issues
Struggling with latch problems can be both painful and frustrating, often leading to more frequent nursing sessions and sore nipples. Ensuring a proper latch from the start makes breastfeeding smoother and more comfortable for both you and your baby.
Some mothers experience pain at the moment the milk starts flowing. This is normal and subsides about a minute later. if sharp pain persists, the next cause is an improper latch. Release the breast from the baby's grasp and try placing them back at the breast. Ensure that the baby opens their mouth wide enough to latch not only onto the nipple but also a portion of its surrounding area—the brown areola. Make sure that the baby's head and body are aligned.
Learn about the proper latch already before your baby arrives and/or get an expert lactation consultant to give you some hands-on support, ideally in the comfort of your own home.
If latch difficulties persist, nipple shields—thin, flexible silicone covers—may provide temporary relief. They can be helpful if:
- You have flat, short, or inverted nipples
- Your baby's small size or weak sucking ability makes it difficult for them to latch properly onto the breast
If using nipple shields, it’s best to gradually transition away from them after about four weeks to encourage natural latching.
Certain physical conditions in the baby, such as a short tongue-tie, can also interfere with an effective latch by restricting tongue movement. If breastfeeding is not going well and other potential issues have been ruled out, it may be worth having a doctor check the baby's tongue-tie.
With time, patience, and practice, finding a comfortable latch becomes easier for both you and your baby. Read about the correct latch and position also in the blog - Everything you need to know about feeding your baby.

Sore, cracked and tender nipples
When you're establishing breastfeeding, your nipples go through a lot of adjustment.
- If your nipples are feeling sore, overly sensitive or get cracked, the first step is to check your baby's latch. A poor latch is often the main cause of nipple discomfort, so ensuring it's correct can help prevent further irritation.
- Try applying nipple cream or lanolin cream to help soothe and heal the skin.
-
Letting your nipples air dry can help
- You may also rub a little breast milk onto the nipples after breastfeeding. Breast milk has natural antibacterial and moisturizing properties that can further aid in healing.
- Once you've addressed latch issues and if discomfort persists, silver nursing cups can provide additional relief. Made from lightweight, medical-grade 925 sterling silver, they offer natural anti-inflammatory and antimicrobial benefits while providing a cooling, soothing effect. You can start wearing them right after birth as a preventive measure or use them as long as you need to ease soreness and promote healing.
Engorgement
This occurs when the breasts become overly full with milk, leading to swelling, pain, and difficulty for the baby to latch. It’s most common in the first few days after birth when your milk comes in (3-7 days), but can happen anytime throughout breastfeeding when milk production exceeds the baby's demand.
- Check breastfeeding position and latch
- Try frequent nursing or pumping to relieve the fullness. However, pump only enough to feel relief, as over-pumping can signal your body to increase milk production.
- Use cold compresses between feeds to reduce swelling. (Chilled cabbage leaves may also serve as a natural remedy to decrease swelling and discomfort—apply them for 20–30 minutes at a time)
- Apply warm compresses or take a warm shower before breastfeeding to help with letdown.
Engorgement is usually temporary and can be relieved by frequent breastfeeding or pumping. Over time, milk production adjusts to demand.
If the issue doesn’t resolve within a few days or you develop a fever, consult your doctor to rule out mastitis and get prompt treatment if needed.

Breast inflammation
Breast inflammation occurs when a milk duct becomes blocked, causing swelling, tenderness, and sometimes redness and warmth around the area. If left untreated, this can progress into mastitis, an infection of the breast tissue.
The solutions are similar to those for engorgement:
- Ensure that your baby latches correctly to promote effective milk drainage and prevent clogged ducts.
- Breastfeed frequently to empty the breast as much as possible.
- Gently massage the affected area under a warm shower to ease discomfort and encourage milk flow.
- If a milk duct is clogged, a gentle massage towards the nipple before and during feeding can help clear the blockage.
- Cooling compresses can help reduce swelling and inflammation.
Mastitis
If engorgement and/or blocked milk ducts persist, it can develop into mastitis, which is an infection of the breast tissue. Mastitis can also occur with nipple cracks, which may lead to an infection due to the spread of bacteria.
With mastitis, the breast becomes hard, hot, red, and painful, and flu-like symptoms such as fever and general malaise may also occur. It's important to seek medical help if symptoms don't improve within 12-24 hours.
In diagnosed mastitis cases, antibiotic treatment may be necessary. It is important to continue breastfeeding or pumping regularly to reduce engorgement, release blocked milk ducts, and prevent further milk buildup.
Rest, drink plenty of fluids, and eat nutrient-rich foods to support your immune system. Also, refer to the recommendations under the subheading for engorgement and inflammation.
Milk Blister
A milk blister is a blocked nipple pore, where skin grows over the opening of a milk duct, trapping milk behind it. It usually appears on the upper part of the nipple as a white-yellowish spot or blister. The pain during breastfeeding can be quite intense.
- It often resolves on its own through the baby's sucking during nursing.
- Place the baby on the breast for a short time – the sucking action can help relieve the blister.
- Try soaking the nipple in saltwater.
- Gently rub the area with a towel. This may help remove the excess skin, opening the pore.
- Pierce the blister with a sterile needle (parallel to the skin); sometimes it helps to break the blister under a warm shower with the edge of your nail.
- Once the blister bursts and milk starts flowing, use nipple cream to heal the skin.
- If possible, immediately place the baby back on the breast to empty the blocked milk duct.

Nipple Thrush
Nipple thrush is a fungal infection caused by Candida albicans, which can make breastfeeding painful. Symptoms may include itching, burning, extreme sensitivity, and nipples that appear bright pink, red, dry, or flaky.
If you suspect thrush, it’s important to see your doctor for the right treatment. Antifungal medication is typically required, and you may also be advised to take probiotics to support your gut health and to avoid the consumption of sugar and white flour.
Thrush can affect both the mother’s nipples and the baby’s mouth. To treat it, both the mother and baby need antifungal treatment, as prescribed by a healthcare provider. Additionally, make sure to sterilize any bottles, pacifiers, and breast pumps regularly to prevent reinfection.
Low milk supply
Low milk supply can be a concern for some moms, but many factors contribute to it, and there are ways to improve it.
Common causes of undersupply:
- Milk production is driven by supply and demand. If you're not breastfeeding frequently enough or if your baby’s latch isn’t effective, your body may not receive the signals to produce more milk.
- Conditions such as PCOS (Polycystic Ovary Syndrome), thyroid disorders, or a history of gestational diabetes can interfere with milk production by affecting your hormones.
-
Some mothers experience delayed lactation due to pregnancy or birth complications. Hormonal imbalances as well as a history of insufficient breast tissue growth, can contribute to this.
- Stress or exhaustion can negatively impact milk supply.
- If you introduce formula or use a bottle too early, it can reduce the baby’s demand for breast milk, which may lower your supply.
Solutions to improve milk supply:
- Make sure your baby is latching correctly and feeding regularly. Aim for at least 8–12 feeds in a 24-hour period. The more your baby feeds, the more milk your body will produce.
- If your baby isn’t nursing efficiently, use a breast pump after feedings to help stimulate milk production.
- Some herbs like fennel, fenugreek and alfalfa are known to support milk supply. Always consult with your healthcare provider before taking any supplements.
- Hormonal imbalances or conditions like PCOS, thyroid issues, or gestational diabetes can impact milk supply. If you suspect an underlying health condition, seek guidance from your doctor for appropriate treatment.
- Take care of yourself by finding ways to rest and manage stress. Consider relaxation techniques like deep breathing and meditation, take small breaks throughout the day to recharge.
- Consult with a lactation consultant, who can assess your breastfeeding technique, check your baby’s latch, and offer personalized guidance and support.
Remember that every breastfeeding journey is different, and it’s important to be patient with yourself as you find the best approach for your body and your baby’s needs.
Nipple strike
A "nipple strike" or "nursing strike" occurs when a baby suddenly refuses to breastfeed despite having done so well before. This can be distressing for both mother and baby.
Reasons for a nursing strike:
- The discomfort from emerging teeth can make babies reluctant to latch.
- If the baby is not feeling well, has a sore throat or a stuffy nose, they may avoiding breastfeeding
- Change in routine like returning to work, a new caregiver, or stress in the environment, may affect the baby’s desire to nurse.
- If the milk flow is too fast or forceful, the baby might refuse to latch.
- As babies get older, they can become more distracted by their surroundings, especially when they are exploring new skills like sitting up or crawling.
How to overcome:
- Try to stay calm, nursing strike is usually temporary, and the baby may return to breastfeeding once the issue is resolved.
- Offer the breast frequently, even if the baby refuses, continue offering without force.
- To maintain milk supply, pump or express milk during the strike.
- Changing nursing positions or feeding location can sometimes make a difference.
- Ensure that there is no illness, teething pain, or discomfort affecting the baby.
- Offer cuddling and reassurance, as the baby may seek comfort over food.
Nursing strikes typically resolve with time. If the strike lasts several days or you're concerned, consult a lactation consultant or healthcare provider.

Cluster feeding
Cluster feeding is when a baby feeds more frequently over a short period, often in the evening, to boost milk supply or for comfort. It can leave the mother feeling exhausted. If the baby's appetite is greater than the current milk supply, it is most likely a growth spurt. By asking to breastfeed more frequently, the baby signals for more milk. This process usually lasts 2-3 days.
- Take rest breaks between feedings.
- Drink plenty of fluids and eat nutritious meals to maintain energy.
- Understand that cluster feeding is often a phase that will pass.
Overactive Letdown
Some mothers may experience a forceful milk flow, which can cause the baby to choke, sputter, or pull away from the breast.
- Try nursing in a more upright position.
- Express a small amount of milk before breastfeeding to slow down the flow.
- Let your baby take breaks during feeds if the milk flow is too fast.
- Use a milk collector or breast pad for the other breast while nursing.
Nipple Confusion
"Nipple confusion" can occur when a baby has difficulty transitioning from breast to bottle and vice versa, as milk flows differently, and the shape and feel of the nipple and bottle teat are different. To avoid "nipple confusion," it is recommended to wait until the breastfeeding is well established before introducing bottles or pacifiers.
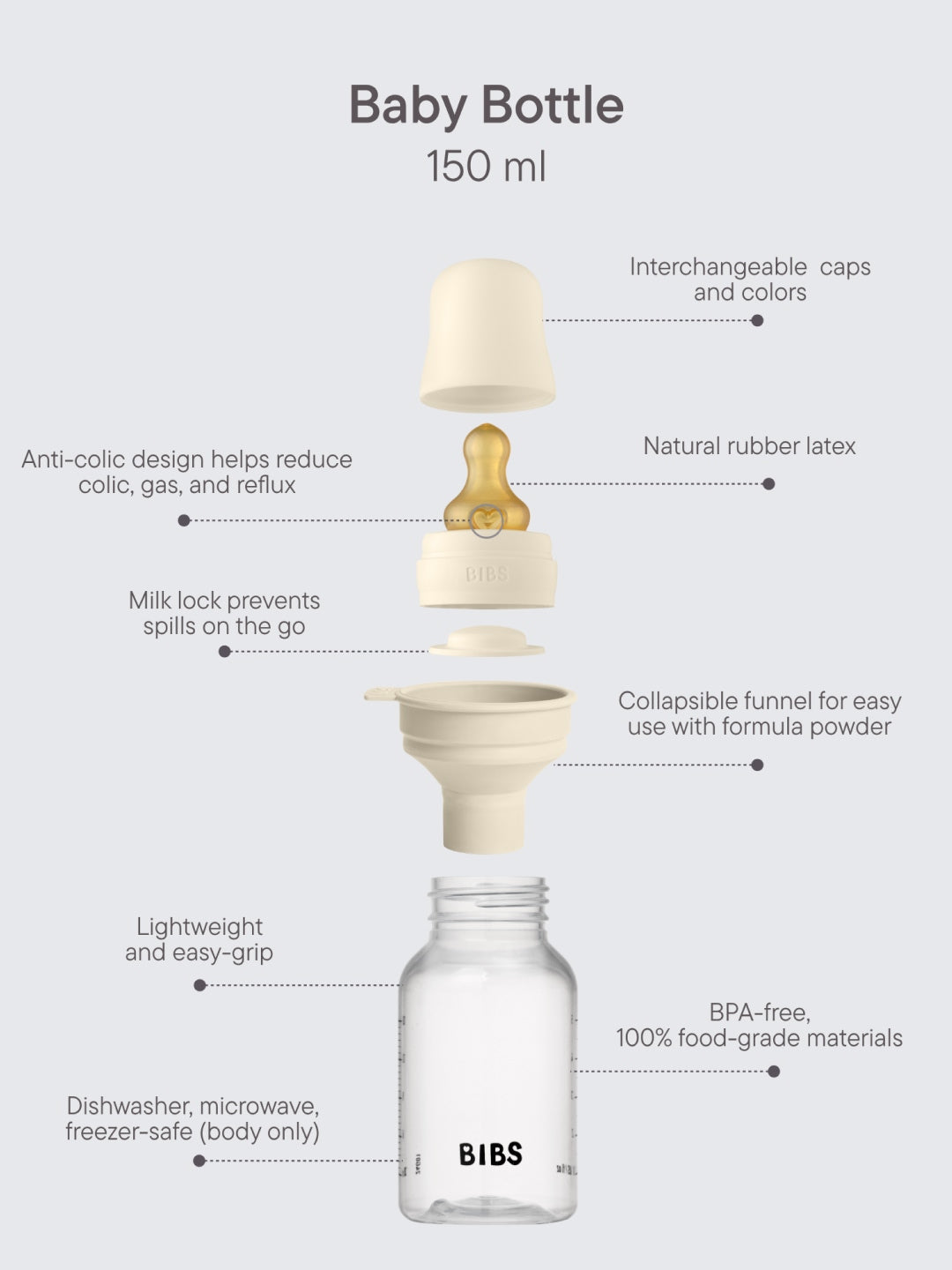
If you do need to use a bottle, paced bottle feeding is a technique that mimics breastfeeding. This method involves holding the baby in a semi-upright position and the bottle horizontally allowing the baby to suck and swallow at their own pace, similar to the flow of milk from the breast. Read more about paced bottle-feeding here.
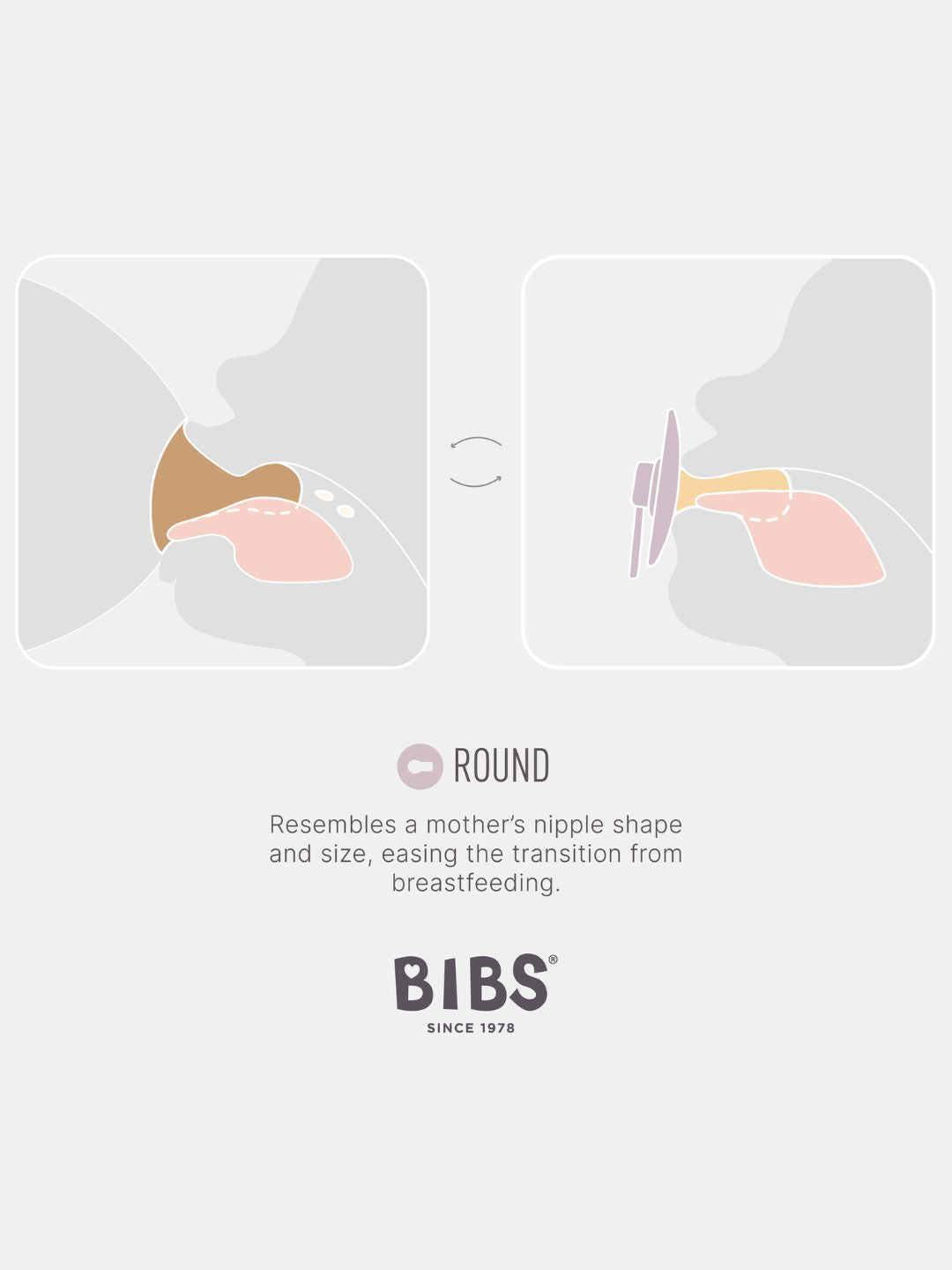
BIBS bottle has round nipple that resembles the shape and size of the mother’s soft nipple and promotes a similar tongue placement and sucking technique as breastfeeding. If your baby is already using a pacifier, use a bottle with a nipple shape similar to the one the baby is already accustomed to. Read more about "nipple confusion" and how to avoid it.
Baby Sleeping on the Breast
This is mainly a concern during the first few postpartum days, until the baby regains their birth weight, or later if the baby is not gaining enough weight.
- Keep the baby in skin-to-skin contact, with only a diaper covering.
- Start feeding from the fuller breast.
- Stimulate the baby to continue sucking by gently tickling the soles of their feet, cheeks, or armpits when sucking slows down.
- After feeding, pump additional milk from the breast for stimulation, as the baby may not fully empty the breast when sleepy, which can decrease milk supply.
- Breastfeed more frequently and wake the baby for feeding at night as well.
Teething
As babies grow and start teething, they may bite or tug on the nipple, causing pain during breastfeeding.
- Try offering a cold teething ring or cloth before breastfeeding to soothe sore gums (there are special teething rings that can be placed in the fridge) and/or use a designated gum gel to relieve gum pain and itching.
- If the baby bites during breastfeeding, gently remove them and calmly offer the breast again.
Food sensitivities or allergies in baby
Some babies may develop discomfort or reactions like rash, excessive crying, or digestive issues if their mother consumes certain foods, such as dairy, caffeine, or spicy foods.
The most common foods that may cause allergic reactions in breastfed babies include cow's milk, eggs, peanuts and tree nuts, wheat, soy, fish and shellfish, citrus fruits.
If the mother notices that her baby has more gas or digestive issues after eating certain foods, it may be helpful to temporarily avoid those foods and monitor if the symptoms improve.
If you suspect a food sensitivity, keep a food diary and consult your pediatrician to determine if dietary changes are needed.
Getting Help from a Lactation Consultant
Breastfeeding can be challenging, especially when you’re experiencing pain, discomfort, or anxiety. If you're struggling, don't hesitate to seek help. A lactation consultant can assess how you’re feeding your baby, including your posture, the way the baby is positioned, and the latch. They can pinpoint areas for improvement and help make breastfeeding feel more natural.
Additionally, the consultant will check your baby for any physical issues, such as a tongue tie, that might be affecting their ability to latch properly and feed comfortably.
If you’re looking for a lactation consultant, ask your midwife or contact the hospital where you gave birth.
Lactation consultations in Estonia:
Pelgulinna Pregnancy and Maternity Center
East Tallinn Central Hospital Women's Clinic
Tartu University Hospital Women's Clinic
Viljandi Hospital
Narva Hospital
Ida-Viru Central Hospital
Rakvere Hospital
Kuressaare Hospital
South-Estonian Hospital
Pärnu Hospital
Järvamaa Hospital
Põlva Hospital
Suun
Sünni ja Imetamise Eesti Tugiühing