If you're hoping to start breastfeeding your baby, learning some essential technique and tools, can help you navigate this new journey — one that may be unfamiliar, occasionally uncomfortable, and undoubtedly exhausting.
Breast milk: a natural start
Breast milk contains all the essential nutrients in proportions that are perfectly suited to your baby’s needs at any given moment. It helps protect the baby against infections, reduces the risk of allergies, and lowers the chances of developing both acute and chronic illnesses, such as cardiovascular diseases later in life. Additionally, breastfeeding decreases the risk of obesity in adulthood. Sucking on the breast soothes the baby, supports oral development, and helps shape a healthy bite.
For mothers, extended breastfeeding offers protection against breast and uterine cancer and may also reduce the risk of chronic conditions like rheumatoid arthritis.
On top of all that, breast milk is always warm, clean, and readily available, which is a significant advantage. It is also the most cost-effective way to nourish your baby. Ideally, no aids are needed for breastfeeding, and the baby can be breastfed practically anywhere.
Breast milk fully meets a baby's need for water, proteins, fats, carbohydrates, vitamins, and minerals until six months of age. A healthy full-term infant does not require any additional fluids or supplements.
The only exception is vitamin D, which is not sufficiently present in breast milk. Therefore, all babies should receive daily vitamin D supplements from the second week of life until the age of two.
The World Health Organization (WHO) recommends exclusive breastfeeding for the first six months of a baby's life and continued breastfeeding alongside complementary foods until at least two years of age or longer.
The first days and the role of colostrum
After childbirth, your body begins to recalibrate its hormones. Pregnancy-related hormones like estrogen and progesterone will decrease, while those responsible for milk production, such as oxytocin and prolactin, rise.
From the moment your baby is placed on your chest for skin-to-skin, their instinct will guide them to latch onto your breast and begin feeding. The first breastfeeding could take place within the baby's first hour of life, as soon as both the mother and baby are ready. It's an amazing display of their natural connection with you during the first moments of life.
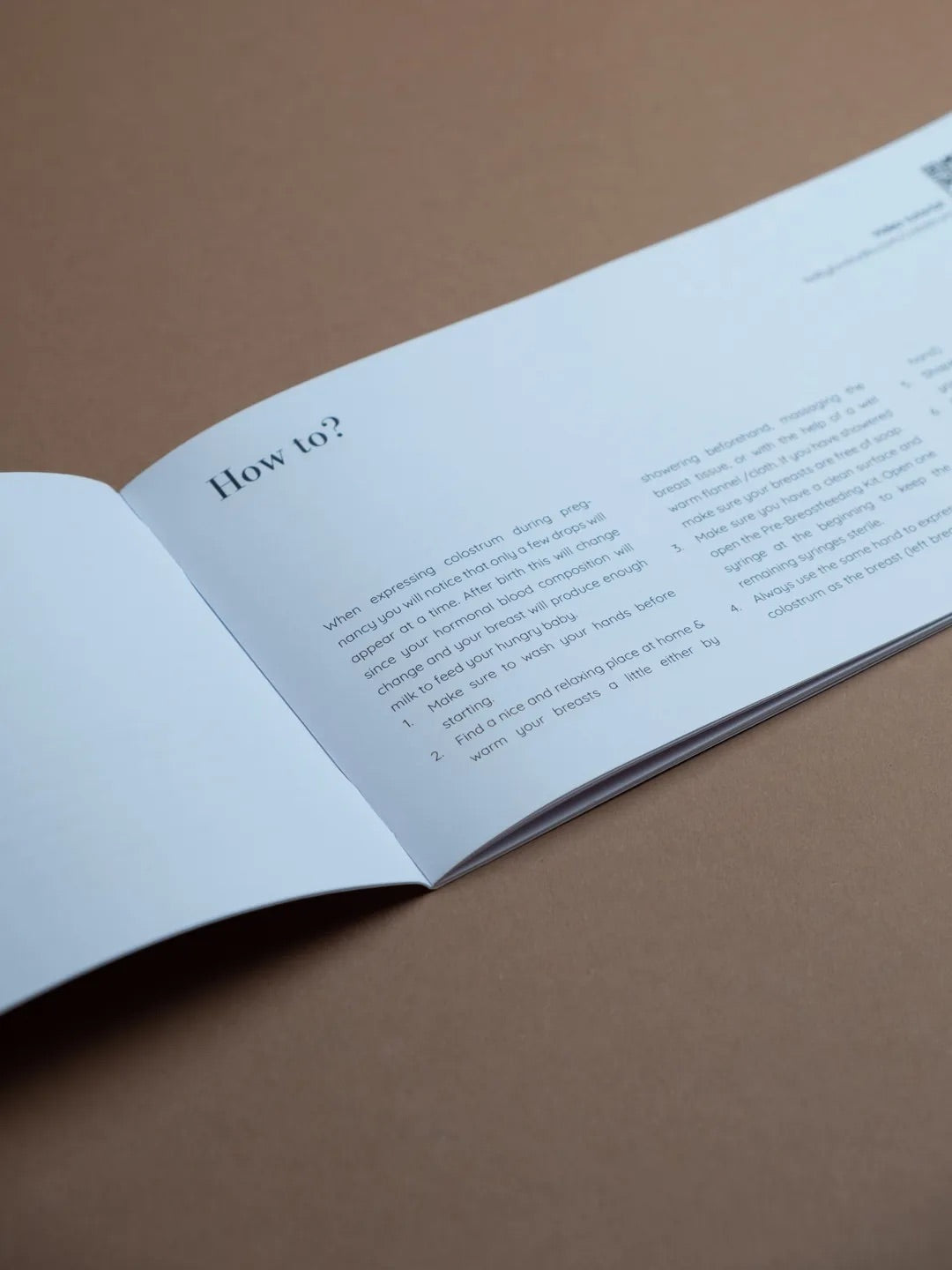
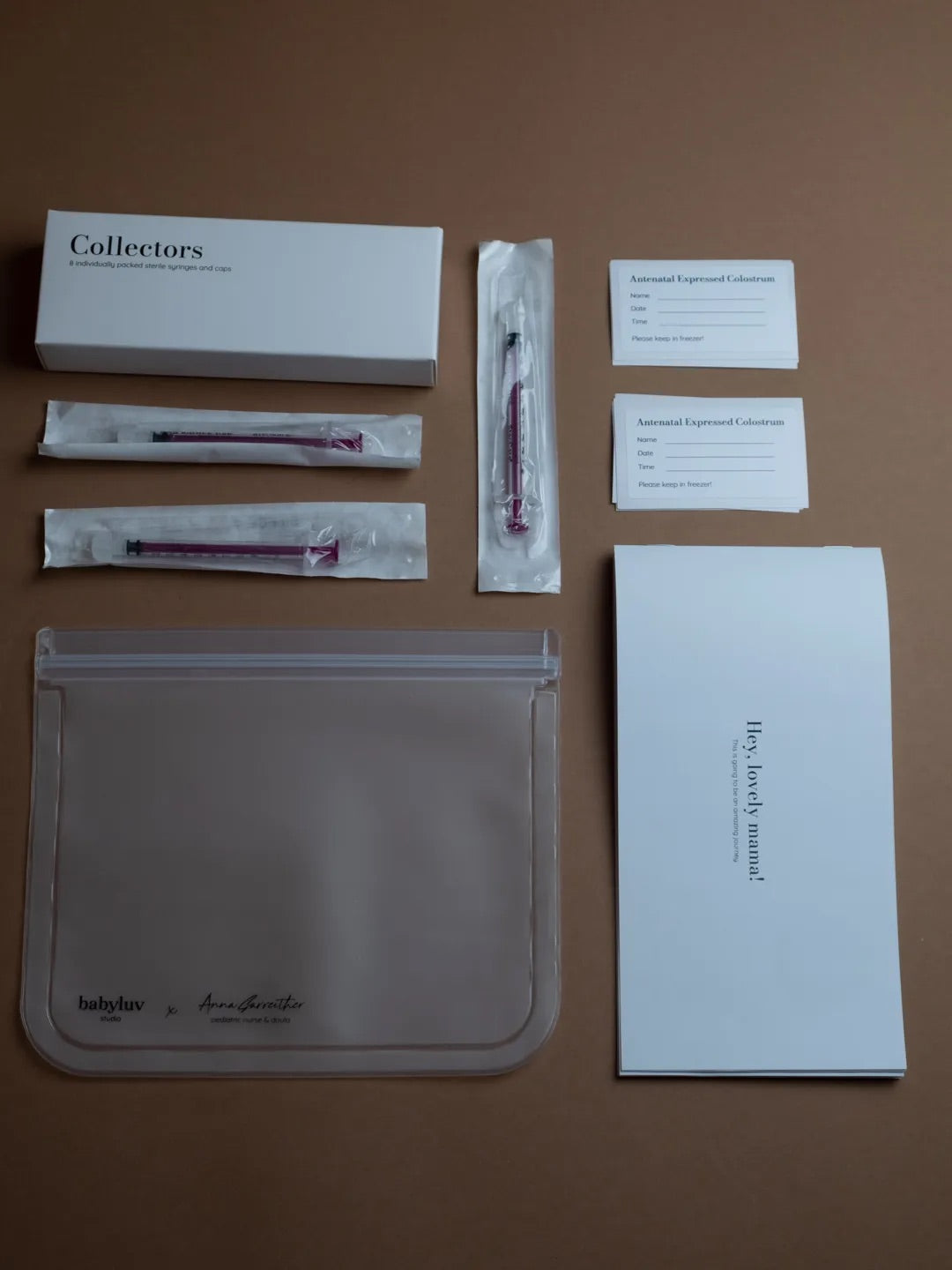
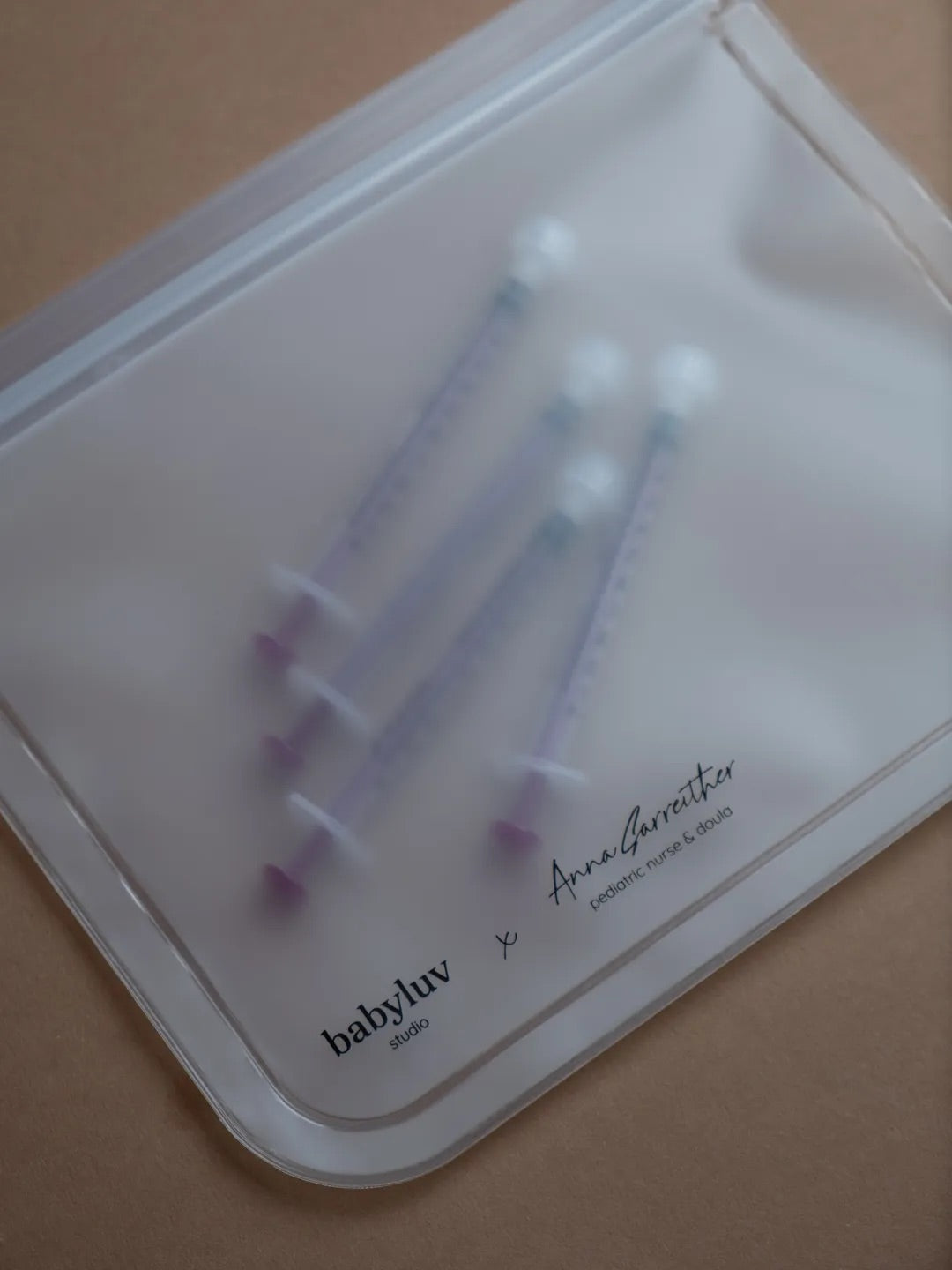
Colostrum is the first form of breast milk. It is gold yellow, packed with healthy fats and protein. Colostrum begins forming in the breasts as early as the 3rd or 4th month of pregnancy, though many women may not notice it, as about half do not experience leaking before birth. You can also start collecting colostrum during pregnancy, but not before 37 weeks, as it may trigger labor. To collect, express it into a sanitized container or use a ready-made kit, and store it in the freezer.
Colostrum is provided to the baby during the first breastfeeding session. After the challenging process of birth, it serves as an excellent energy source for the newborn. Though the amount of colostrum is very small, just one or two teaspoons are enough for the baby’s first day of life, as colostrum is highly concentrated. If you have expressed colostrum, take it to the hospital to use as a supplement during the early days.
Colostrum protects the baby from surrounding germs, activates their delicate digestive system, helps them adjust to life outside the womb, and guards against jaundice.

Transitional milk and mature milk
In the first few days, you may experience cluster feeding, where your baby demands frequent feeds with little breaks in between. This can be exhausting, but it is temporary. More frequent and longer breastfeeding sessions will help increase the milk supply in the breasts. Offer the baby the breast whenever they ask, and let them stay at the breast as long as they wish. The feeding interval should not exceed 3-4 hours in the beginning.
It is normal for the baby's weight to drop in the first few days (the loss should not exceed 10% of the birth weight). If the pediatrician recommends feeding the baby more frequently, the breast should be offered at 2-3 hour intervals.
By days 3 to 5 postpartum, many mothers notice that their breasts become much fuller and firmer as milk production ramps up. This can lead to engorgement, where the breasts feel overly full with milk and uncomfortable. While it can be unpleasant, this is a positive sign that your body is starting to produce more milk.
If the breasts become too full, taking a warm shower before feeding, expressing a little milk to make it easier for the baby to latch, and breastfeeding frequently can help improve comfort. After feeding, apply a cold compress to the breasts to relieve the discomfort.
In the first few weeks, the breasts produce what is known as transitional milk, and the amounts can vary - sometimes there is a lot of milk, sometimes little, and the breasts may feel either too soft or too hard. The mother’s body is still learning and adjusting to the new situation, which is why it is very important to feed according to the baby's cues, so that the breasts "learn" to produce milk according to the baby's needs. Full or mature milk is typically produced only after the sixth week postpartum.
When your baby starts nursing, your body releases oxytocin, triggering your milk ducts to release stored milk - this is called letdown reflex. As milk flow increases, your baby settles into a natural sucking rhythm.
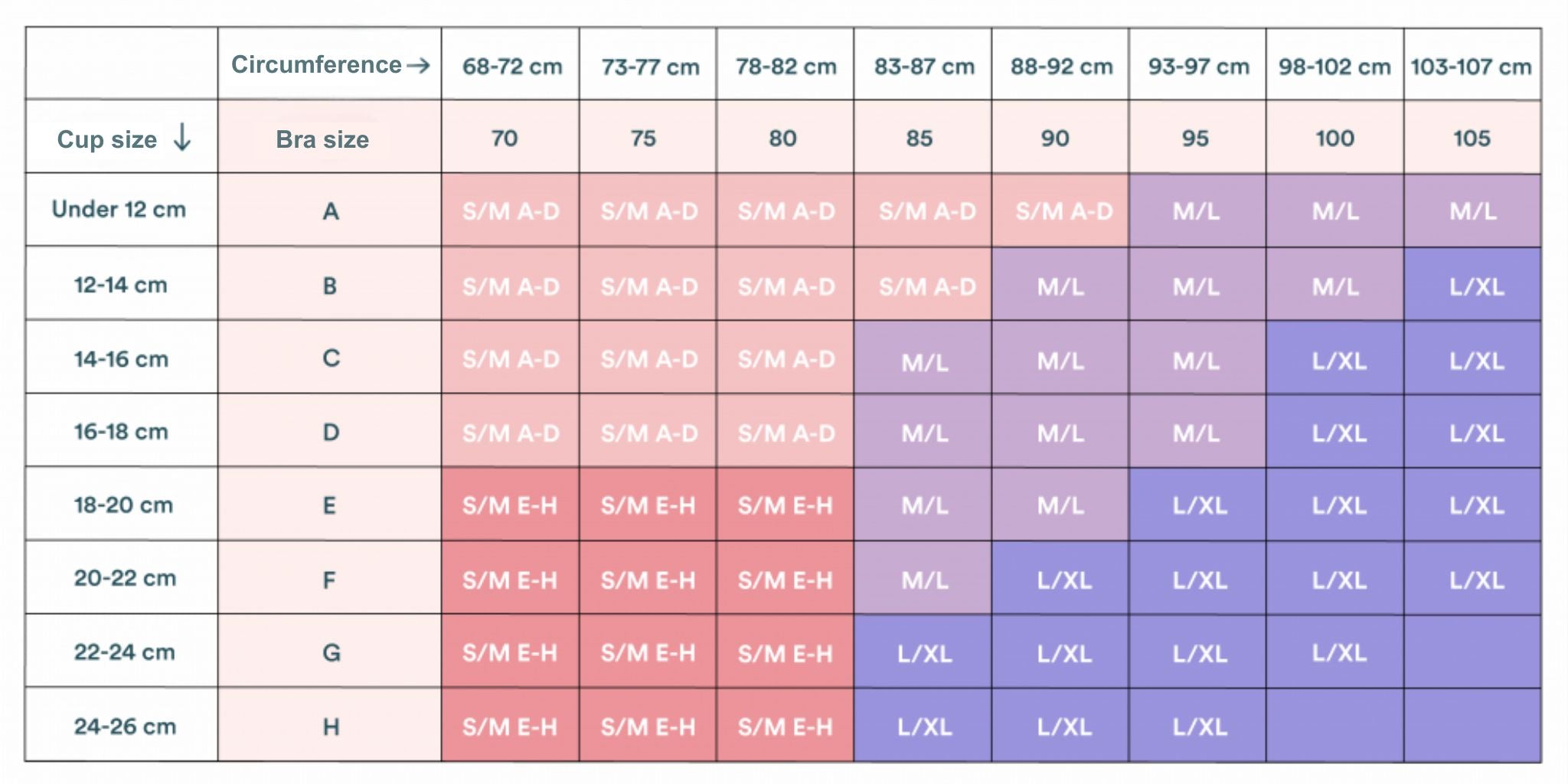
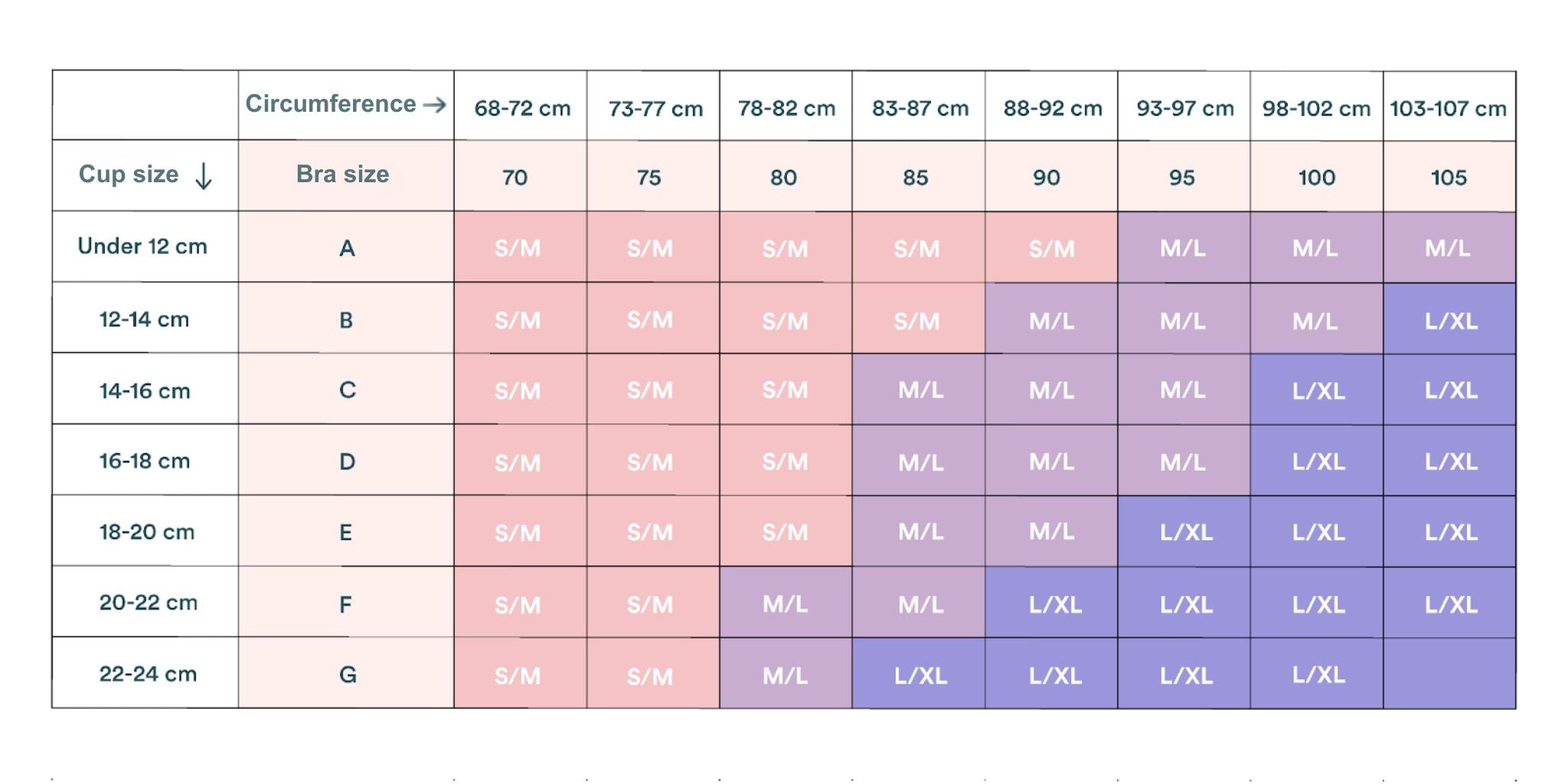
Letdown usually happens within the first minute of feeding but can occur earlier - just hearing your baby cry or preparing to nurse may trigger it. If milk leaks before your baby latches, absorbent breast pads can help. You can also use a milk collector to catch any milk leaking from the other breast while feeding. Easily opened, soft and stretchy nursing bra makes the whole process more comfortable.
Adjusting and finding a comfortable routine
Breastfeeding in the early days can be challenging as you find a routine that works for both you and your baby. Pain, frustration, and discomfort are common, and many mothers feel overwhelmed and as if they’re failing. Know that this is normal and not a reflection of your love or efforts. Breastfeeding takes time and practice.
As breastfeeding becomes more established, your breasts will adapt to your baby's needs, and fullness will ease. In the first few weeks, feeding on demand - typically 8 to 12 times in a 24-hour period - is normal as you and your baby find a rhythm. It can take up to 8 weeks for your milk supply to regulate and meet your baby’s specific needs.
However, some women may still face challenges, such as low milk supply, cracked nipples, mastitis, or conditions in the baby like tongue tie. If this is the case, reaching out to a lactation consultant can help resolve issues and ease discomfort.
Read also a blog about common breastfeeding problems and solutions.

Mastering the latch
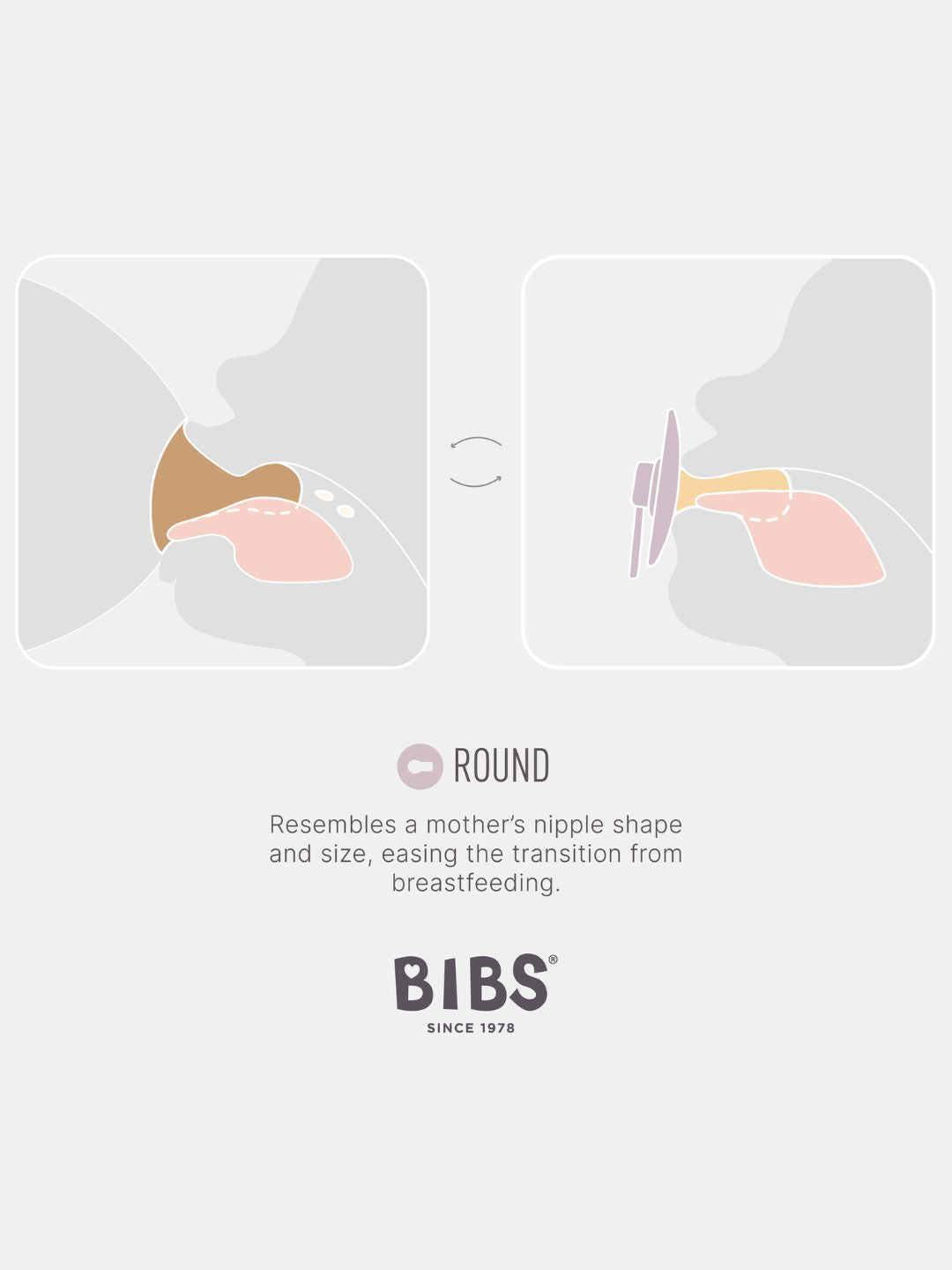
The latch refers to how your baby fits over the nipple and the breast. It’s a key to comfortable and effective breastfeeding. A good latch not only helps your baby get enough milk, but also ensures you’re comfortable throughout the process.
How to achieve a proper latch:
- Position your baby breast height, facing the nipple, allowing them to latch.
- Gently bring your baby close, tummy against your tummy, keeping their head and body aligned.
- Ensure their cheeks press symmetrically into the breast, with their chin tucked in and nose aligned with the breast.
- The upper and lower lips should be turned outward (you can gently help with your finger if needed), creating a slight double chin.
- Ensure your baby opens their mouth wide enough to cover not just the nipple but also a good portion of the areola. A shallow latch can lead to nipple pain and poor milk transfer.
Signs of a good latch include:
- Comfort without pain.
- Consistent rhythmic sucking, and audible swallowing sounds.
- After feeding, your baby should appear satisfied and well-rested, while your breasts should feel softer.
The baby will release the breast when full or when it’s empty. Always offer the other side - if still hungry, they’ll continue feeding; if not, they won’t. This ensures they get exactly what they need for growth and development.
After breastfeeding, the baby should be burped to release any swallowed air. Hold the baby in an upright or semi-upright position until they burp, then place them on their side to sleep.
If you’re experiencing sharp pain or if your nipple looks misshapen or flattened after breastfeeding, your baby may not be latched properly. A proper latch should feel like gentle pulling or tugging without pain.
If latch issues persist or cause discomfort, it’s always a good idea to reach out to a lactation consultant. They can offer personalized guidance, check the latch, and recommend techniques or solutions to make breastfeeding more comfortable and effective.

The importance of posture
Proper posture is essential while breastfeeding. Comfort is crucial for both. While a good latch can ensure your baby is feeding properly, it’s also important for you to feel relaxed and comfortable. Slouching or sitting awkwardly can strain your back. If you’re tense, it can affect the feeding process.
It's helpful to try different positions, whether lying in bed, semi-reclined or sitting, to see which one works best for both of you.
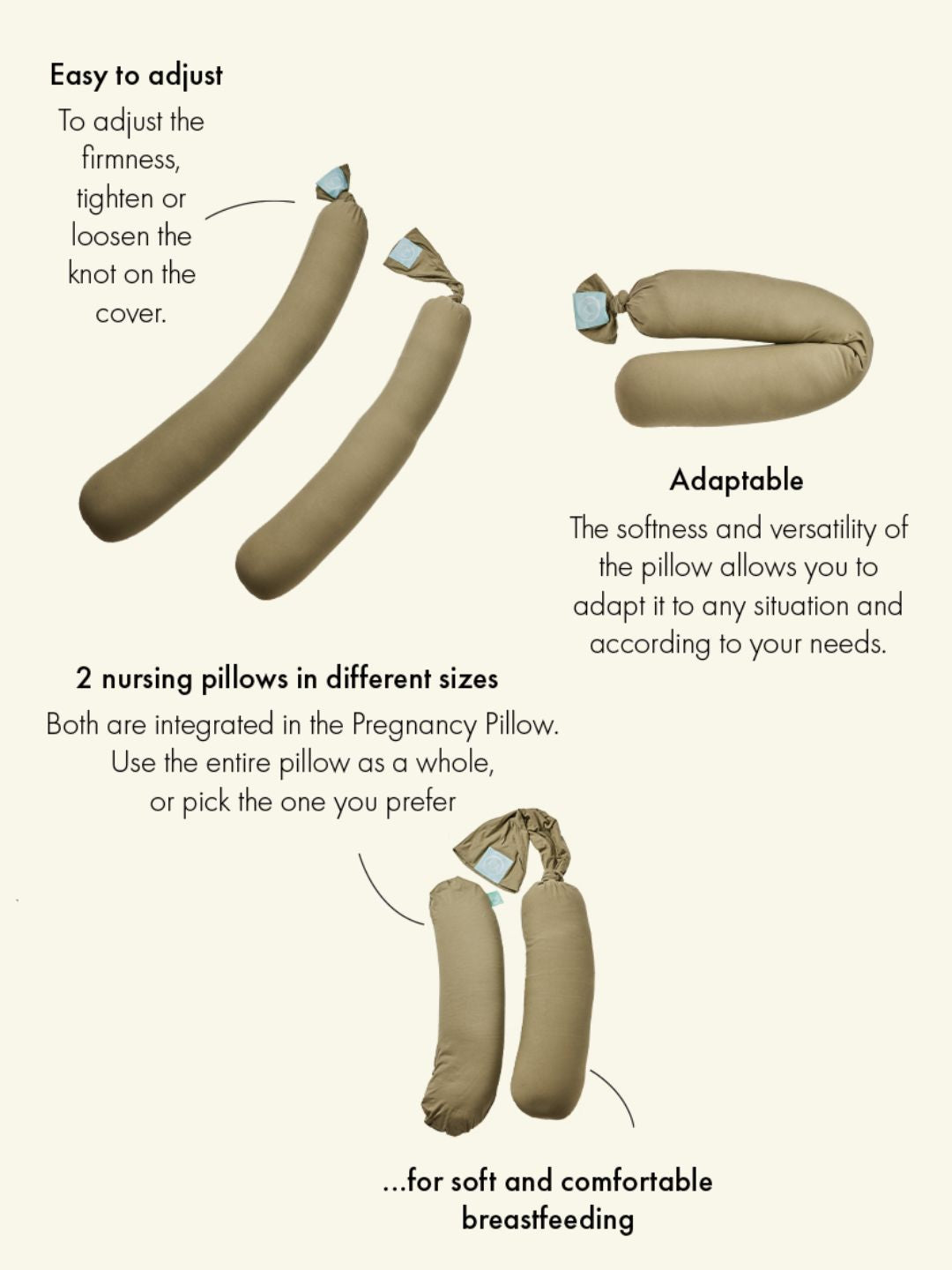
In the beginning, a lying position may feel more comfortable, allowing you to rest while feeding. In a semi-reclined or sitting position, use a nursing pillow that supports your arms and back, allowing your shoulders to stay relaxed. The pillow helps position the baby at breast height during breastfeeding and support comfortable feeding position.
The feeding position you choose should prioritize both your comfort and your baby’s ability to feed effectively.
Managing discomfort while breastfeeding
If you're new to breastfeeding, it's normal to experience some nipple sensitivity, dryness, or roughness as your body adjusts. Your nipples are adapting to a completely new function, and you’re likely still figuring out the most comfortable position and latch. Using a special nipple cream can help soothe and protect the skin, easing some of the initial discomfort.
Additionally, taking a warm shower before feeding, expressing a little milk to make latching easier, breastfeeding frequently, and applying a cold compress to the breasts after feeding can all help improve comfort and relieve discomfort.
However, not all pain is normal. Trust your instincts - if something feels off, don’t hesitate to seek advice from a healthcare professional.
Read a separate blog article about common breastfeeding problems and solutions.
Nutrition and hydration during breastfeeding
Breastfeeding is demanding on the body, using up to 500 extra calories a day. To keep your energy up and support milk production, focus on nutrient-rich foods and eating balanced meals.
Prepping easy, one-handed snacks like nuts, fruit, and lactation cookies can be a lifesaver during busy days. Freezable meals are also a great way to make sure you have nourishing food on hand when sleep is scarce. Don’t hesitate to ask friends and family to bring a meal when they visit.
Hydration is just as crucial - aim to drink 2–3 liters of fluids daily. Breast milk production averages around 750 ml per day during the first six months, increasing a breastfeeding mother’s fluid needs by approximately 600-700 ml per day. To stay hydrated, drink water and herbal teas. Ask your partner or support person to refill your water bottle throughout the day, and always have a drink and a snack when feeding your baby.
A good-quality postnatal vitamin can help fill any nutritional gaps.
A breastfeeding mother should avoid carbonated sugary drinks, products containing preservatives and colorants, as well as spicy and strongly flavored foods. A mother with a fussy baby is advised to consume caffeinated drinks in moderation, not more than two cups a day.

Getting help from a lactation consultant
Breastfeeding can be challenging, especially when you’re experiencing pain, discomfort, or anxiety. If you're struggling, don't hesitate to seek help. A lactation consultant can assess how you’re feeding your baby, including your posture, the way the baby is positioned, and the latch. They can pinpoint areas for improvement and help make breastfeeding feel more natural.
Additionally, the consultant will check your baby for any physical issues, such as a tongue tie, that might be affecting their ability to latch properly and feed comfortably.
If you’re looking for a lactation consultant, ask your midwife or contact the hospital where you gave birth.
Lactation consultations in Estonia:
Pelgulinna Pregnancy and Maternity Center
East Tallinn Central Hospital Women's Clinic
Tartu University Hospital Women's Clinic
Viljandi Hospital
Narva Hospital
Ida-Viru Central Hospital
Rakvere Hospital
Kuressaare Hospital
South-Estonian Hospital
Pärnu Hospital
Järvamaa Hospital
Põlva Hospital
Suun
Sünni ja Imetamise Eesti Tugiühing
Feeding your baby, your way
Breast milk is the optimal source of nutrition for infants, but there are situations where breastfeeding may not be possible or recommended due to medical reasons affecting either the mother or the baby.
Additionally, breastfeeding is not always easy, and some mothers may encounter challenges in starting or continuing to nurse. In such cases, infant formula provides a suitable alternative during the baby’s first year.
For many parents, choosing how to feed their baby is a deeply personal decision. Whether you continue breastfeeding, pump and bottle-feed, or use formula, all are valid and healthy choices. If breastfeeding doesn’t work out or isn’t the right fit for you, nobody should judge that. The most important thing is to make a choice that supports both your baby’s well-being and your own needs.
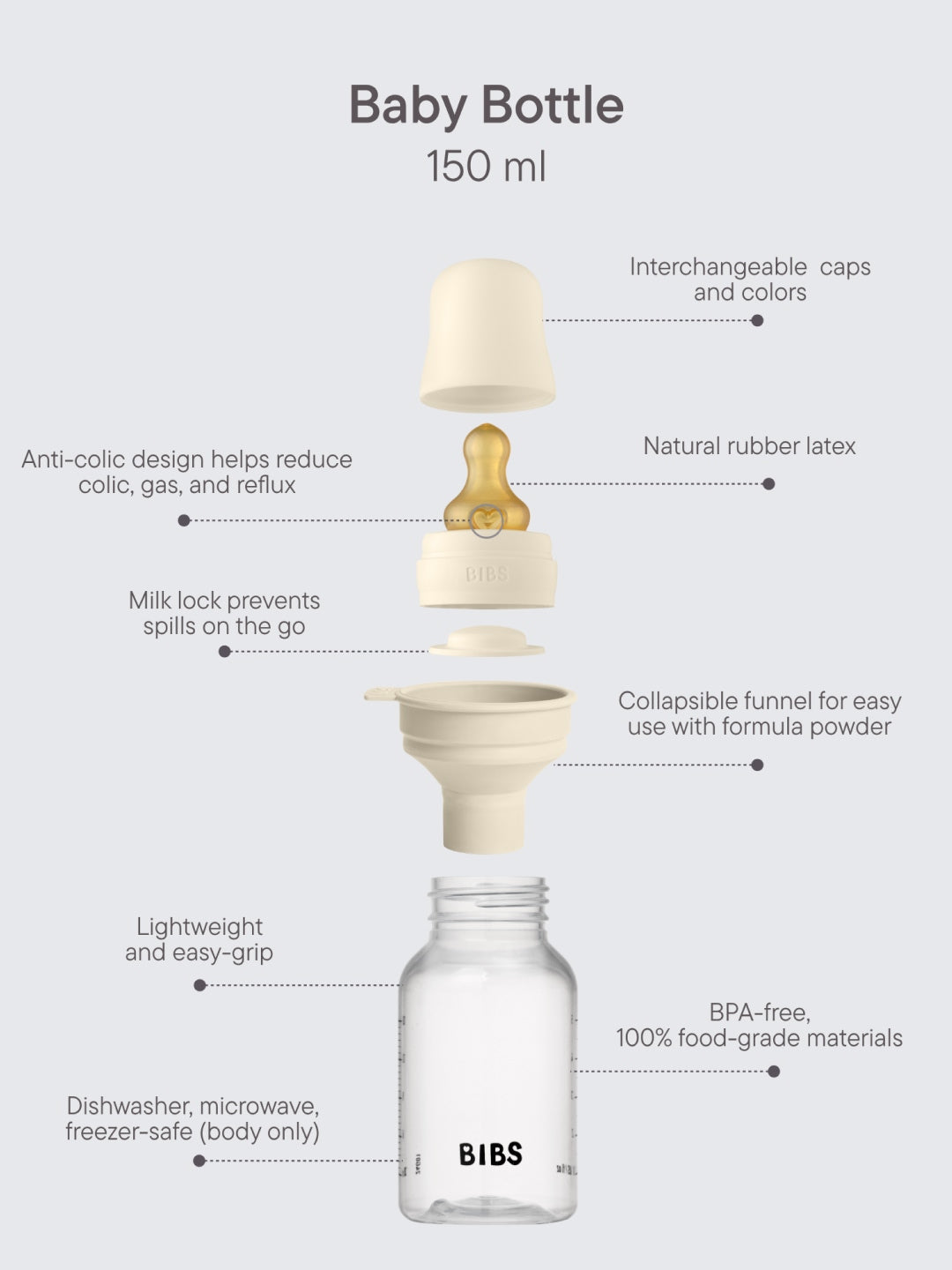
Also bottle-feeding - whether with formula or expressed breast milk - ensures that your baby receives the necessary nutrition to grow and thrive. Your mental, physical, and emotional health matter too, and you are the best judge of what works for you and your baby.
At the end of the day, what matters most is that your baby is fed, cared for, and loved. Whether you breastfeed, bottle-feed, or combine both, you are making the best choice for your family. It’s not just about breastfeeding - it’s bestfeeding.